Peripheral vein (IV) equipment management
- Share
- From
- BQ+ medical marketing
- publisher
- Michael
- Issue Time
- Jun 4,2022
Summary
University teacher and student team's visiting and study in BQ+ Medical

Peripheral vein (IV) equipment management
introduce
Peripheral venous catheter (PIVC) is the most commonly used intravenous device in hospitalized patients. They are primarily used for therapeutic purposes, such as drug administration, infusion and/or blood products, and blood collection.
The target
The purpose of this guide is to provide an outline for the ongoing maintenance and management of PIVC for patients in hospitals, outpatient clinics, and home medicine Settings. Refer to the venous access guide for information on PIVC insertion. Nurses deemed competent to perform IV insertion may continue PIVC insertion after consultation with the NUM/CSN.
The terms defined
Peripheral venous infusion device: A cannula/catheter inserted into a small peripheral vein for therapeutic purposes, such as medication, infusion and/or blood products.
Aseptic techniques: are part of all procedures designed to prevent pathogenic microorganisms sufficient to cause infection from entering susceptible critical sites through critical sites, hands, surfaces and equipment. Thus, unlike aseptic techniques, standard and surgical aseptic techniques are possible and can be implemented in typical hospital and community Settings.
Hand disinfection: Perform hand hygiene to protect patients from organisms that may enter their key parts or equipment during surgery.
Key component: Part of the equipment that must remain sterile throughout the clinical process. Examples of critical components include catheter joints, needle-free joints, syringe joints, needles, etc.
Critical site: Areas on the patient's body, such as the intravenous injection site, must be protected from microscopic organisms.
Extravasation: Extravasation occurs when foamed drugs or fluids accidentally penetrate into the tissue surrounding the venipuncture site.
Infiltration: Occurs when drugs or fluid penetrate the tissue surrounding the venipuncture site. This happens when the tip of the catheter slips out of the vein and the catheter extends through the vein wall or blood vessel wall, allowing fluid to inject into the surrounding tissue.
Phlebitis: Signs of damage to blood vessels. The cause may be chemical (due to osmotic pressure from the solution), mechanical (from trauma during insertion or movement) or infectious (microbial contamination of the equipment). Signs include swelling, redness, fever, induration, suppuration, palpable venous cords (hard veins), and pain associated with local inflammation of the vein at or near the insertion site.
Infusion pumps: Infusion pumps, such as large volume pump (LVP)/ volume pump, such as Alaris Signature Edition (SE), syringe driver (such as Alaris GH+), patient-controlled Analgesia /PCA pump (Alaris PCAM) etc.
Double examination: The practice of two clinicians (appropriately approved registered nurse (EN), registered nurse (RN), physician, or pharmacist) independently reviewing medications.
assessment
Patient and IV site assessments should be performed periodically.
The PIVC assessment includes:
Evaluation of PIVC insertion site - catheter position, patency/occlusion, limb symmetry, any signs of phlebitis (erythema, tenderness, swelling, pain, etc.), infiltration/extravasation. PIVC is considered to be a high risk of stress injury. Unless otherwise recorded, the PIVC site should be examined hourly for pressure ulcers and any signs of infection. http://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Pressure_Injury_Prevention_and_Management/.
Evaluation of PIVC dressings and splints: Check the fixation of the dressing -- whether it is intact, clean, dry, loose or if there is visible exudate under the dressing. Check whether the plywood tape is too tight or too tight.
Evaluation of IV pipelines, equipment and IV fluids:
If the patient is receiving a continuous IV fluid infusion, the IV site, infusion type and volume, the patient's exact infusion rate, and infusion pump pressure alerts are observed hourly and recorded on the fluid balance flow chart.
If the patient (in hospital setting) is receiving intermittent infusion, a minimum of 8 hours of evaluation is required. More frequent evaluation of unstable patients with signs and symptoms of complications.
If the patient no longer needs INTRAVENOUS fluids, remove the cannula as soon as possible to avoid complications.
For home-based hospital (HITH) patients, the nurse will evaluate PIVC at each visit.
Caregivers and patients will be educated on signs of injury and the process of contacting nurses.
management
Intravenous infusion, drug infusion, or administration of blood products
A) Continuous infusion of intravenous fluids
Evaluation and recording of results should be completed hourly to determine effective delivery of prescription medications and fluids.
Each bag of fluid is independently double-checked and a signed patient label is affixed to the bag.
Check whether the solution is the specified solution, infusion speed and infusion volume.
Record infusion volume: every hour on the fluid balance flowchart (it is recommended to clean infusion pump every hour)
Check the infusion site for any signs of complications and record the assessment hourly on the fluid balance chart
Review cumulative infusion and fluid output as needed, based on the patient's clinical status.
Pump pressure for each IV line shall be recorded hourly or as adjusted on the flow chart
Infusion pump pressure
Default pressure limits for intravascular infusion pumps are programmed by biomedical engineering according to manufacturer recommendations.
Upper infusion pump pressure can be manually increased according to clinical judgment to accommodate:
Increased liquid viscosity
High infusion rate
The diameter of the intravascular catheter decreases
The length of the intravascular catheter increases
Increase the patient's activity level
Check PIVC for patency if pump pressure exceeds recommended limits.
B) Push injection/load dose administration:
Administration of drugs:
Drugs administered via PIVC may be
Diluted into a bag of I.V. fluids
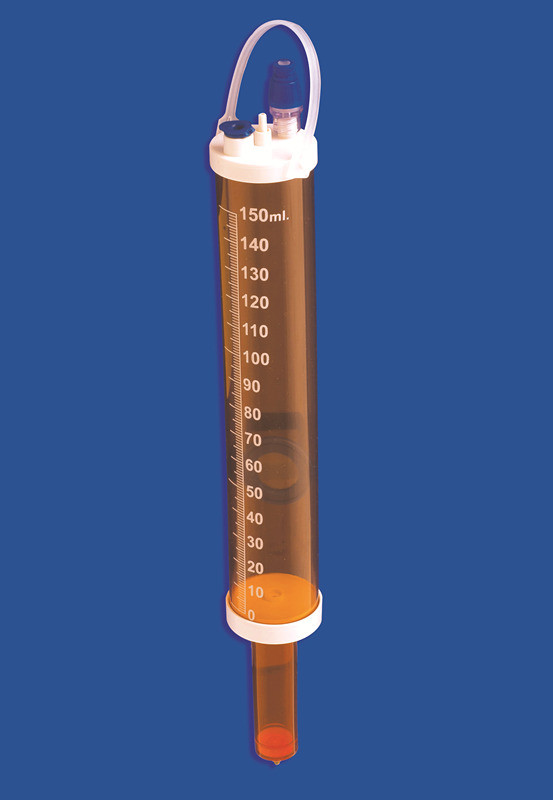
Add to burette of infusion set
Prepare to administer through a volumetric infusion pump
Used in syringes for syringe drivers
Administer directly as a push or push injection
The most appropriate method should be selected based on the volume of diluent required, patient condition, fluid balance and expected delivery speed.
A drug administered by:
Infusion burette: Dilute the drug to a smaller volume through the burette feeding system, hang the infusion bag, gradually open the roller holder, and let the right amount of diluent into the burette. Fill prescription drugs into burette through additive port.
Syringe driver: Recommended for children weighing less than 10 kg. Draw the required volume of diluent into an appropriately sized syringe and then pull back the syringe plunger to enable you to inject the drug into the syringe using aseptic techniques.
Infusion bag: Clean the inlet of the infusion bag with a sterilized cotton swab before injecting the prepared drug through the additive port. Insert the spikes on the dosing device into the diaphragm of the infusion bag without contaminating the key component (spikes).
Attach a complete drug label detailing the drug, dosage, diluent, diluent volume, date, time, and the signature of the nurse and staff who examined it carefully.
PIVC can only be accessed after cleaning the access port and scrubbing the hub.
For intermittent infusions, the disconnected IV line will be discarded between infusions. Once the dosing device is disconnected from the casing, be sure to flush the casing with normal saline. For opioid infusion booster, see specific guidelines: Pediatric Pain Management Services (CPMS) (Opioid Infusion Guidelines)
Management of blood products:
Check the patient and blood product labeling according to blood product transfusion procedures.
Manage the infusion of blood products through volume infusion pumps or syringe drivers to ensure accurate delivery. Gravity devices are used only when rapid dosing is required and capacity is closely monitored.
Neonatal infusion sets (including the 170 to 200 micron filter required for blood products) and syringe drivers are used to deliver small amounts of blood products.
Using aseptic contact-free techniques, the septa of blood products is spiked with a neonatal infusion set and an appropriately sized syringe is connected to a 3-way faucet.
Draw the desired volume into the syringe and fill the rest of the neonatal infusion set. Label the syringe with patient and blood product identification details, including the expiration date and time of the blood product.
If a small amount is needed for rapid infusion, the desired amount is sucked into the syringe through a 170 - to 200-micron filter.
Burette should not be used in blood transfusions.
PIVC washing
If the tube is used intermittently for administration or infusion, the tube should be flushed before infusion or at least once per shift.
The catheter should be flushed with sterile 0.9% sodium chloride for injection. This must be prescribed as a medication.
The optimal volume for intermittent injection or infusion is not known. The literature recommends that the volume of irrigation be at least twice the volume of the catheter and the attachment device, and that at least 2mL of normal saline be used for irrigation.
Rinse with a 10ml syringe to avoid excessive pressure and catheter rupture. Syringes with a diameter less than 10mL can create higher pressure in the lumen and cause catheter rupture. If resistance is felt and pressure is applied during flushing, this may cause extravasation
Use aseptic non-contact techniques, including vigorously cleaning the access port (scrubbing the hub) with a double disinfectant (e.g. chlorhexidine and alcohol) for at least 15 seconds and allowing it to dry before entering the system.
Rinse with pulsating (push stop) action.
Flushing catheter:
Immediately after placement
Before and after infusion (due to lack of infusion pressure in an empty fluid container, blood will flow back into the catheter lumen from normal venous pressure) or injection.
Before and after blood drawing.
Replace PIVC dressing and fixed sleeve:
Dressing at the PIVC site is the first line of defense against infection and displacement. Dressings must be kept safe, clean, dry and in good condition.
Indications for dressing change: when it becomes unsafe or there is leakage of blood or fluid under the dressing.
Prior to surgery, the need for an assistant was determined considering the patient's age, level of development, and family involvement.
If the patient is allergic to clear film dressings, use a sterile film dressing and change it daily.
Carefully remove the old dressing and always secure the cannula in place
Take this opportunity to thoroughly inspect the casing entry site for any signs of infection.
Skin preparation with 2% chlorhexidine alcohol is the preferred solution for dressings.
Clean the area around the insertion site, including under the hub, using a mode that ensures coverage of the entire area.
Allow the skin to prepare to air dry before applying any dressings to allow the disinfectant to take effect.
Consider placing a small sterile cotton ball or gauze under the intubation hub to relieve pressure.
If required, place sterile tape over the hub of the equipment before placing a clear dressing.
A sterile transparent semi-permeable sealing dressing (e.g. Tegadermtm, IV 3000TM) placed over the catheter using sterile contactless techniques covers the site of cannulation insertion. This will allow continuous observation of the site and help stabilize and fix the catheter.
IV plates/splints are recommended to secure PIVC placed in or near the buckling area. This will fully immobilize the joint and minimize the risk of venous injury due to flexion.
When using splints, make sure they are placed and tied to the limbs and fingers in a neutral position to prevent injury by restricting blood or nerve supply and to prevent pressure sores
Check the splint at least once a day and replace it if it is stained by blood or fluid leaks.
Cover with a non-compression tubular bandage. Ensure that there is a clear window for intubation into the skin insertion site so that the site can be viewed periodically.
In conclusion, when trimming the peripheral IV cannula, ensure that:
It's safe
The website is visible
The child must not harm himself or be harmed by the connection
The child cannot remove or move the casing
Tape is not too tight or restrictive.